Calculating Work Burden in an Acuity Matrix
Posted on: August 10th, 2009Calculating work burden in an acuity matrix
Work Burden is a measure of the difficulty and effort required to deliver care. It is a measure pioneered by Workforce Prescriptions, Inc. as an alternative to less flexible measures of productivity. It begins with the development of a custom Acuity Model.
An Acuity Model categorizes individual patient care needs based on risk, complexity and skill level required by providers. It accurately provides both the clinician and leadership with valuable information on the needs of care in a specific environment and the complexity/burden that such care demands.
Constructing a customized acuity model requires 3 key steps:
- Creation of an acuity grid
- Assigning of Skill requirements to the grid
- Determining a Scoring Methodology for “Work Burden/Work Intensity”
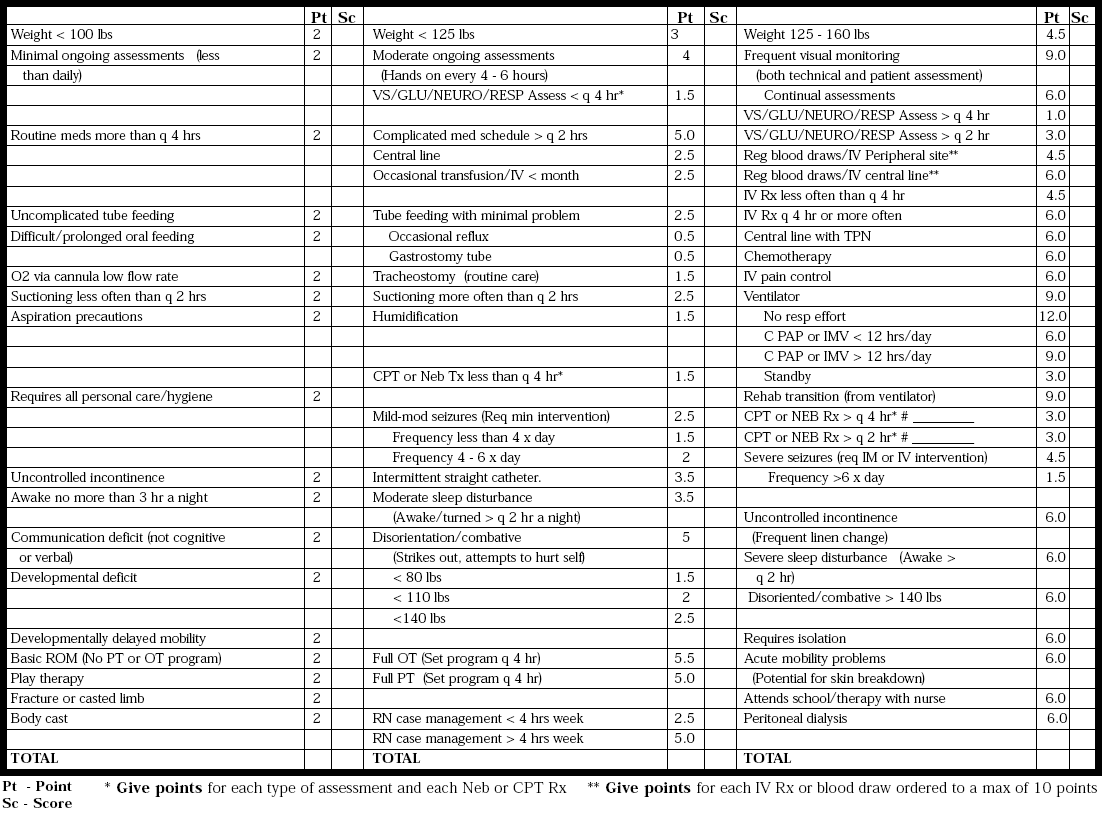
STEP 1: Creating a Grid
Building an acuity model always begins with the creation of an “Acuity Grid” (See Below). The purpose of the grid is to allow each care area to define independently the types of presenting conditions, the effort co-efficient of each and how multiple diagnoses can stack to create greater complexity in the delivery of care. Acuity, seen through the lens of distinct organizations can mean different things for identical diagnosis. Points shouldn’t be based on just the generally recognized “level of acuteness” but rather on three important factors (which can change from hospital to hospital, department to department):
- How far away needed supplies are (supplies necessary to providing the care associated with a particular DRG)
- How sick the patient is as a baseline (are there other issues at play that may not rise to the level of a DRG but do impact complexity of care, IE advanced age, inability to participate in care decisions, etc . . .)
- The general availability of needed equipment (that may need to be “shopped for”)
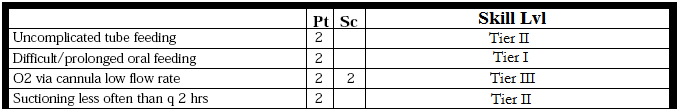
STEP 2: Assigning Skill Requirements to the grid
The next thing that occurs in constructing an acuity model is the overlaying of skill requirements to the diagnosis/issues detailed in the grid (SEE BELOW). The purpose of this is not to perform a “time and motion study” of effort and skill – rather to outline basic skill levels as they relate to the actual requirements of care.
Many organizations collaborate with the clinical educators in each area and apply a clinical ladder assessment to each diagnosis in order to solidify both the value of their clinical ladder and to begin to “invigorate it” by identifying the
specific proficiencies tied to each level.
Step 3: Determining a Scoring Methodology for “Work Burden/Work Intensity”
Every organization eventually creates its own mathematics around “Work Burden”. Often this number becomes a greater factor in determining budgets than inaccurate or non-comparable industry data of “worked hours per volume”, FTE’s per AOB, etc . . . When overlaid with volume and census data, work burden calculations provide operational and financial leaders with a level of understanding of the resource requirements that are actually impacting the character and difficulty of work for care givers.
The goal of a Work Burden calculation is to ensure that variances in labor are reconciled with the changes in workload created by short and long term changes in acuity, volumes and churn (number of turns per labor hour). It can also be used as the basis for redefining how care is distributed among members of a care team (Senior RN’s, Junior RN’s, NA’s, Techs, LPN’s, etc. . .). The calculation follows:
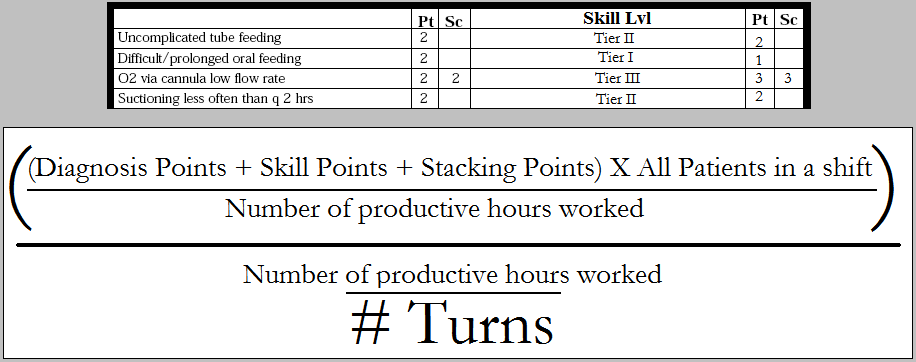
A sample Work Burden calculation*:
In this sample, a unit on day shift accumulated 283 points for diagnostics, skill and stacking (all patients during the 8 hour shift). 6 RN’s did all the work and they logged 46 productive labor hours during the shift. There were 9 bed turns during the shift. The Work Burden calculation would be:
283 points/46 productive Hrs = 6.15 = 1.20
46/9 5.11
If this same unit on the following day had the same volumes but 6 more turns and much higher acuity requiring the utilization of another 8 labor hours, the equation could look like this:
371 points/54 productive Hrs = 6.87 = 1.91
54/15 3.60
So even though patient volumes stayed the same and work hours went up – the proof of productivity is in the clearly increased work burden. This is valuable in helping:
- Managers to understand how work is “feeling” to their staff and why
- Nursing supervisors to optimize scheduling around patient care needs
- Nursing and Operational leaders redesign how care is delivered and workflow is designed
- Financial leaders to optimizing coding and billing as well as practice patterns
- Organizations to improve patient satisfaction by optimizing and aligning care delivery
*Collaboration with finance is a MUST when developing a work burden calculation as a component of acuity management. Assumptions of difficulty in acuity must be established collaboratively and benchmarking of “standard work burden” must be accomplished over a 2 quarter period to ensure appropriate calibration.
View All Articles